Patrick Arbuthnot was browsing his emails on what seemed like a normal workday in his lab in Johannesburg when he saw a strange notification pop up.
“Stop Work,” it read.
Arbuthnot does not remember exactly what else the United States official said in the body of text in January, but the one line seared in his memory was enough, even if it was almost impossible to believe.
For two years, the researcher had worked on developing an HIV vaccine to possibly help put an end to one of Africa’s most deadly diseases for good. His lab at South Africa’s University of the Witwatersrand (Wits) had already spent thousands of dollars in US funding on experiments. Now, all of that crucial work had to be paused – or worse, permanently halted.
“It’s all such a waste, it’s all such a waste. Those were the words that kept running in my head when I saw the message,” Arbuthnot, who directs Wits’s Antiviral Gene Therapy Research Unit, told Al Jazeera, months after the nightmare unfolded. “It seemed like it was all just for nothing.”
Dozens of health trials across Africa were forced to grind to an abrupt halt in late January after US President Donald Trump pulled the plug on millions of dollars in funding without warning. His executive order paused aid to developing countries provided through the US aid agency, USAID, and PEPFAR (the US President’s Emergency Plan for AIDS Relief), pending a three-month review period. The cuts swept across programmes tackling a host of deadly diseases in Africa, particularly malaria and HIV.
Southern African countries, with the most HIV cases globally, had leaned heavily on the US to fight the pandemic. With the cuts, HIV clinics serving vulnerable populations like sex workers and MSMs (men having sex with men) suddenly shut down. Health workers lost their jobs in the thousands. People living with HIV were unsure of how to access crucial medication. Poorer countries like Zimbabwe, where USAID funded about 80 percent of the HIV response, were so badly hit that even condom supplies were disrupted.
For African scientists racing to get HIV under control, the timing could not have been worse.
Barely days before, Arbuthnot had met with other researchers working on similar trials at a conference in Zanzibar. They’d all left the breezy island feeling positive.
“We had the pasta in the boiling water, and we were just waiting for it to [cook],” the scientist said, illustrating how far his vaccine trials had gone before the stop-work order was issued. “There was still work to do to get the pasta ready. You still had to mix it with your sauce, so it wasn’t quite ready to eat yet, but we already had the pasta in the water. We were getting there.”
 A pharmacist holds a vial of lenacapavir, an injectable drug to treat HIV, at the Desmond Tutu Health Foundation’s Masiphumelele Research Site, in Cape Town, South Africa [Nardus Engelbrecht/AP]
A pharmacist holds a vial of lenacapavir, an injectable drug to treat HIV, at the Desmond Tutu Health Foundation’s Masiphumelele Research Site, in Cape Town, South Africa [Nardus Engelbrecht/AP]Progress halted
Since 2023, Arbuthnot has received funding from the US to create preventive vaccines by sequencing the genetic makeup of two “elite controllers”, a rare group of HIV-infected people who are somehow able to lead normal lives without using antiretrovirals (ARVs) to suppress their viral loads.
The two people in Arbuthnot’s trial are anonymous – identified simply as CAP 255 and CAP 25 – but they form part of a group whose condition researchers see as something of a superpower, as they do not develop symptoms or seem to need medication.
Arbuthnot’s trial is part of the US-funded Brilliant Consortium project, which features African researchers from more than seven countries, including Nigeria, Zimbabwe and Kenya, all racing to develop vaccines and highly effective HIV preventive or management therapy.
Such gene sequencing work in Africa is also crucial to help understand how diseases affect people from the continent. So far, Africa’s human genomes make up only 2 percent of the total sequenced human genomes.
Africa has the most HIV cases of any continent, and South Africa accounts for the largest number of infections – nearly 8 million people. Experts say a toxic combination of apartheid-era labour and segregation policies, low incomes, and deep mistrust of Western healthcare institutions is to blame.
It’s why HIV studies are heavily concentrated in South Africa, more than in any other African nation. Because HIV patients have weakened immune systems prone to tuberculosis (TB), research into both diseases often goes hand-in-hand.
World leaders pledged in 2016 to end AIDS by 2030, and African scientists appear eager to deliver the cure.
But creating an HIV vaccine, like Arbuthnot is trying to do, is incredibly difficult because of how fast the virus mutates and how well it disguises itself once inside a host’s DNA. Despite decades of studies, progress has been limited, partly because funding is limited.
With crucial US funding now cut, the entire sector has been thrown into disarray, and progress, experts say, has been rolled back.
PEPFAR is credited with allocating a significant portion of the $100bn it has donated since 2003 to African countries. In South Africa, it supported as much as 18 percent of the HIV budget. Scientists, in a recent study, found that shutting down PEPFAR would result in more than 600,000 HIV-related deaths and half a million new infections in South Africa alone, over the next 10 years.
“It’s not just the fact that the funding was cut that was the problem,” Esther Casas, an HIV-TB adviser at medical NGO Doctors Without Borders, known by its French initials MSF, told Al Jazeera. MSF does not rely on US funding and is still running its HIV centres, but everyone across the board was affected one way or another, Casas said.
“It was the sudden way it [the US funding cuts] was done. To do something like that, you have to prepare the people. But that did not happen, and that was catastrophic,” she said.
 Lab technician Xolile Mhlanga works with vials of lenacapavir. Twice-yearly shots of the drug used to treat AIDS were 100 percent effective in preventing new infections in women, according to study results [Nardus Engelbrecht/AP]
Lab technician Xolile Mhlanga works with vials of lenacapavir. Twice-yearly shots of the drug used to treat AIDS were 100 percent effective in preventing new infections in women, according to study results [Nardus Engelbrecht/AP]Lenacapavir: The breakthrough drug
It was not only trials and experiments that the US cuts disrupted. Trump’s orders have also affected real, tested, and more effective pre-exposure prophylaxis (PreP) therapies achieved after years of trials.
PreP is what prevents people at risk of exposure to HIV – like partners of people living with HIV – from being infected. Common forms of the medication are daily pills that some people may find hard to stick to, and with efficacies of between 74 and 99 percent.
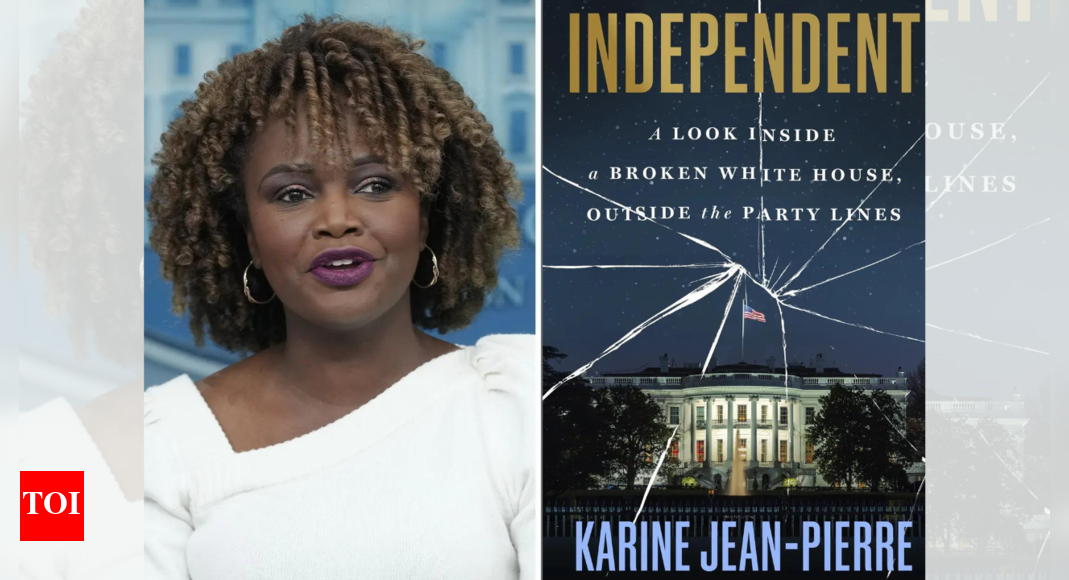
Last year saw a rare breakthrough in the form of lenacapavir, a PreP drug tested on 5,000 young women between the ages of 16 and 25 in South Africa and Uganda. It was 100 percent effective. It was also more convenient: Patients required only two shots every six months.
Although the trials were funded by Gilead Pharma, a US biopharmaceutical company, USAID was planning to step in for the next important step: Helping to take lenacapavir to generic drug makers who would make it available on the market at affordable prices.
“Now, that pipeline is completely gone,” Nomathemba Chandiwana, chief scientific officer at the Desmond Tutu Health Foundation in Cape Town, told Al Jazeera. Her boss, Linda Gail-Bekker, who directs the nonprofit research centre, was a principal investigator in the trials.
After the Trump administration’s stop-work order, some projects received notices that their funding would be reinstated, but others, like the lenacapavir project, are still unsure where they stand.
“Can you imagine? This was the biggest thing to happen in HIV, the scientific breakthrough of last year, and now we don’t have a path forward,” Chandiwana said.
Expecting the South African government to carry the burden of getting lenacapavir on the market is not realistic, the scientist added. The drug is expensive, she said, and the Department of Health might struggle to provide the budget.
‘Not all doom and gloom’
As the US aid cuts delivered shock after shock to Africa’s health systems and HIV care response in particular, critics blamed African governments for overreliance on aid and pointed to the billions of dollars lost in large-scale corruption scandals in the two biggest economies: Nigeria and South Africa. Both countries, until January, received about a fifth of their HIV response budget from Washington.
Casas of MSF said the turbulence is certainly a wake-up call for Africans to take full responsibility for their healthcare, from research to drug development and treatment. Yet it will take years to understand how deep the disruptions caused by the US may go, she said, adding that it is way too much power for any single external entity to wield.
“We cannot afford to allow access to healthcare, access to HIV and TB care, and other conditions affecting the most vulnerable communities to be politicised. We must realise that the solution and response will probably not come from any one funder,” said Casas.
Arbuthnot is among a few lucky researchers who have managed to secure other avenues of funding. Since the US pulled out, the US-based charity, ELMA Foundation, has stepped in to support his lab’s work. Things remain uncertain, though, as the funding is only for six months.
Despite having a real, instant effect on people’s lives, some African researchers say doing their work is starting to feel impossible. Chandiwana said other countries, including the United Kingdom, are rolling back research funding even as critical research work shuts down due to internal politics and priorities.
“Our work is not abstract at all. It’s not like ‘oh, whatever’ kind of work,” Chandiwana said. “We are shrinking as a community, but the health problems we are tackling are getting bigger and bigger.”
The task for African health scientists going forward, experts say, will be how to involve their governments, and how to use less money to deliver life-saving results. Some governments appear ready for the journey: Nigeria, in February, released $200m to immediately plug the funding gaps. In South Africa, an additional $1.5bn was added to the health budget.
At the Desmond Tutu Foundation, Chadiwana said one way she and her and colleagues are coping is by diversifying focus and including more non-communicable conditions like obesity in their research. That will help add more options to the funding basket, she said.
“The changes are scary, but in the times of dragons, you need dragon slayers,” Chadiwana said of how scientists should adapt. “I am an eternal optimist, so it’s not all doom and gloom. We just have to keep at it.”

 1 month ago
20
1 month ago
20









 English (US) ·
English (US) ·